
Blog
Bronchiectasis unveiled: Causes, symptoms & how clinical research can help

AUTHOR
Olivia Ustariz
Date Published
27 November 2023
Overview
Can you imagine being plagued by a loud, mucusy cough for months, if not years on end? What about being perpetually breathless, with the threat of lung infections looming constantly over your head? Unfortunately, this is the reality for people living with bronchiectasis, a chronic lung condition where the bronchi are irreversibly damaged and can lead to recurrent chest infections.
Though there is currently no cure for bronchiectasis, researchers are working hard to uncover more about this condition and develop potentially life-changing therapies. In this blog post, we will delve into the world of bronchiectasis and discuss a new clinical trial that could advance bronchiectasis care and ensure a brighter future for everyone affected by this condition.
What is bronchiectasis?
Bronchiectasis is a chronic lung condition that occurs when the bronchi, the tubes that connect the lungs to the windpipe, are abnormally and irreversibly widened - usually due to long-term inflammation and/or infection. In a vicious cycle, this irreversible damage allows mucus to pool in the airways, subsequently leading to ongoing infections and inflammation.
Causes
There are several conditions that can cause bronchiectasis, including:
- Pertussis, which is more commonly known as Whooping cough.
- Severe pneumonia.
- Tuberculosis.
- Cystic fibrosis and other conditions that can affect a person’s ability to clear mucus from their airways.
- Autoimmune conditions and chronic inflammatory diseases that affect connective tissue, such as rheumatoid arthritis, Crohn’s disease, and inflammatory bowel disease.
- Fungal infections and allergic bronchopulmonary aspergillosis (ABPA), an allergic reaction to the fungus called aspergillus.
- Chronic obstructive pulmonary disease (COPD), which is the umbrella term for a variety of diseases that can cause airflow blockage and make it hard to breathe, including emphysema and chronic bronchitis.
These conditions can damage the airways and prevent them from clearing mucus, a naturally occurring substance that traps dust and other small irritants and helps the body expel them through coughing. This build-up of mucus can subsequently become infected and lead to recurrent chest infections.
Though the prevalence of bronchiectasis is not accurately known, it has a high prevalence among Indigenous communities, females, and the elderly (according to the Bronchiectasis Toolbox).
Symptoms
The most common symptom of bronchiectasis is a chronic cough with sputum - a mixture of saliva and mucus. Other symptoms can include:
- Sinusitis - inflammation of the sinuses.
- Wheezing or shortness of breath.
- Haemoptysis - coughing up blood.
- Chest pain.
- Fatigue.
- Recurrent chest infections, known as ‘flare ups’.
Diagnosis & treatment
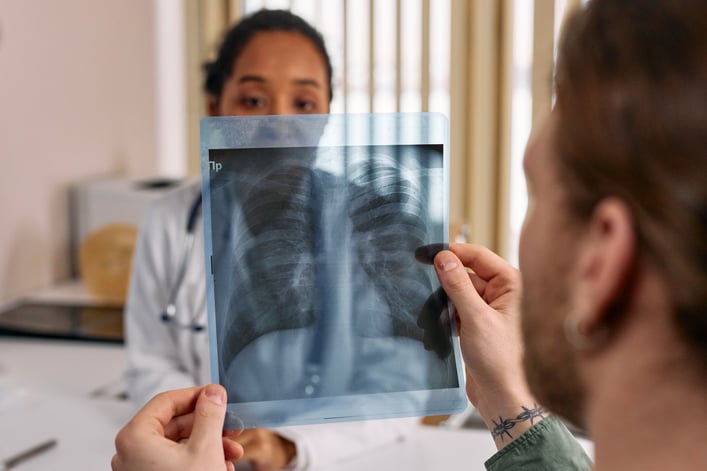
As bronchiectasis shares symptoms with several other lung diseases, it is important to visit your GP for a formal diagnosis, which may include:
- Asking about your symptoms and overall health.
- Listening to your breathing with a stethoscope.
- Looking at your lung tissue and airways in detail via a chest x-ray or high resolution CT scan.
- Testing a sample of your sputum for bacteria or fungi.
- Testing your blood for infections or other possible causes.
- A lung function test to check how well your lungs are working.
Currently, there is no cure for bronchiectasis, so early treatment is vital for controlling infections, improving how you feel, and preventing further lung damage. Some treatment options include:
- Antibiotics.
- Bronchodilators, a type of medication that relaxes the muscles in the lungs, widens the airways, and makes it easier to breathe.
- Inhaled corticosteroids, which help reduce inflammation, the activity of the immune system, and sputum production.
People with bronchiectasis can also self-manage their symptoms without the need for specific medications, including:
- Working with a physiotherapist to develop a daily program of physical exercises, breathing exercises, and coughing exercises that make it easier to clear sputum.
- Quitting smoking.
- Taking care of your overall health by exercising regularly, eating well, and getting plenty of rest, as this can help reduce the symptoms of fatigue, dyspnoea (laboured breathing), and ultimately improve your quality of life.
- Following up regularly with your team of healthcare professionals and staying up to date with your vaccinations for influenza and pneumococcal disease.
- Bolstering your emotional health by joining a support group, doing the things you love, and spending time with friends and family, as people with bronchiectasis have an increased incidence of anxiety and depression.
How clinical research can help
As you can see, bronchiectasis presents unique challenges when it comes to treatment options, in that patients must work closely with their healthcare team and follow an elaborate regimen of medication, rehabilitation, and self-care techniques to manage their symptoms.
As such, clinical trials provide an exciting avenue to improve our understanding of bronchiectasis, its causes, and to ultimately find more effective treatment options. At time of writing, we are currently recruiting for a clinical trial investigating a potential new treatment for bronchiectasis.
By participating in this clinical trial, you could not only change the course of your own healthcare journey, but also contribute to potentially ground-breaking therapies that empower the bronchiectasis community.
To find out more about this study, and other respiratory studies for which we are currently recruiting, visit our website.